What is glaucoma?
Glaucoma is a disease of the optic nerve – the part of the eye that carries the images we see to the brain. The optic nerve is made up of many nerve fibers, like an electric cable containing numerous wires. When damage to the optic nerve fibers occurs, blind spots develop. These blind spots usually go undetected until the optic nerve is significantly damaged. If the entire nerve is destroyed, blindness results.
Early detection and treatment by your ophthalmologist (Eye M.D.) are the keys to preventing optic nerve damage and blindness from glaucoma. Glaucoma is a leading cause of blindness in the United States, especially for older people. but loss of sight from glaucoma can often be prevented with early treatment.
What are the different types of glaucoma?
Chronic -open-angle glaucoma: This is the most common form of glaucoma in the United States. The risk of developing chronic open-angle glaucoma increases with age. The drainage angle of the eye becomes less efficient over time, and pressure within the eye gradually increases, which can damage the optic nerve. In some patients, the optic nerve becomes sensitive even to normal eye pressure and is at risk for damage. Treatment is necessary to prevent further vision loss. See a short video on Open Angle Glaucoma.
Typically, open-angle glaucoma has no symptoms in its early stages, and vision remains normal. As the optic nerve becomes more damaged, blank spots begin to appear in your field of vision. You typically won’t notice these blank spots in your day-to-day activities until the optic nerve is significantly damaged and these spots become large. If all the optic nerve fibers die, blindness results. Follow this link to a short video on Glaucoma and Blind Spots.
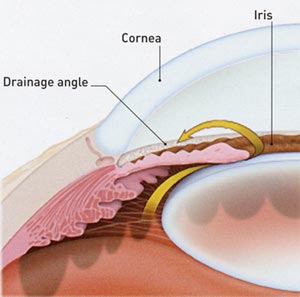
Closed-angle glaucoma: Some eyes are formed with the iris (the colored part of the eye) too close to the drainage angle. In these eyes, which are often small and farsighted, the iris can be sucked into the drainage angle and block it completely. Since the fluid cannot exit the eye, pressure inside the eye builds rapidly and causes an acute closed-angle attack.
This is a true eye emergency. If you have any of these symptoms, call your ophthalmologist immediately. Unless this type of glaucoma is treated quickly, blindness can result. Unfortunately, two-thirds of those with closed-angle glaucoma develop it slowly without any symptoms prior to an attack. See a short video on Closed Angle Glaucoma.
Who is at risk for glaucoma?
Your ophthalmologist considers many kinds of information to determine your risk for developing the disease. The most important risk factors include:
Follow this link for more detailed information regarding the Visual Field Test for Glaucoma.
Photography of the optic nerve or other computerized imaging such as Optical Coherence Tomography may be recommended. Some of these tests may not be necessary for everyone. These tests may need to be repeated on a regular basis to monitor any changes in your condition.
Loss of vision can be prevented
Regular medical eye exams can help prevent unnecessary vision loss. Recommended intervals for eye exams are: