Diabetic Retinopathy – What is it and how is it detected?
Diabetes can affect sight
If you have diabetes mellitus, your body does not use and store sugar properly. High blood-sugar levels can damage blood vessels in the retina, the nerve layer at the back of the eye that senses light and helps to send images to the brain. The damage to retinal vessels is referred to as diabetic retinopathy.
Types of diabetic retinopathy

Normal Fundus
There are two types of diabetic retinopathy:
- nonproliferative diabetic retinopathy (NPDR)
- proliferative diabetic retinopathy (PDR)
NPDR, commonly known as background retinopathy, is an early stage of diabetic retinopathy. In this stage, tiny blood vessels within the retina leak blood or fluid. The leaking fluid causes the retina to swell or to form deposits called exudates. See a short video on Nonproliferative Diabetic Retinopathy (NPDR).
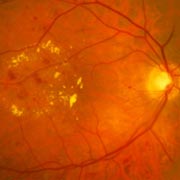
NPDR showing blood and yellow exudates in the macula.
Many people with diabetes have mild NPDR, which usually does not affect their vision. When vision is affected it is the result of macular edema and/or macular ischemia.
Macular edema is swelling, or thickening, of the macula, a small area in the center of the retina that allows us to see fine details clearly. the swelling is caused by fluid leaking from retinal blood vessels. It is the most common cause of visual loss in diabetes. Vision loss may be mild to severe, but even in the worst cases, peripheral vision continues to function. Read more about Cystoid Macular Edema.
Macular ischemia occurs when small blood vessels (capillaries) close. Vision blurs because the macula no longer receives sufficient blood supply to work properly. See a short video on Macular Edema and Macular Ischemia.

PDR showing growth of numerous abnormal blood vessels at risk for bleeding. Without treatment, this patient is at high risk of vision loss.
PDR is present when abnormal new vessels (neovascularization) begin growing on the surface of the retina or optic nerve. The main cause of PDR is widespread closure of retinal blood vessels, preventing adequate blood flow. The retina responds by growing new blood vessels in an attempt to supply blood to the area where the original vessels closed.
Unfortunately, the new, abnormal blood vessels do not resupply the retina with normal blood flow. The new vessels are often accompanied by scar tissue that may cause wrinkling or detachment of the retina.
PDR may cause more severe vision loss than NPDR because it can affect both central and peripheral vision. See a short video on Proliferative Diabetic Retinopathy (PDR).
Proliferative diabetic retinopathy causes visual loss in the following ways:
Vitreous hemorrhage: The fragile new vessels may bleed into the vitreous, a clear, jelly-like substance that fills the center of the eye. If the vitreous hemorrhage is small, a person might see only a few new dark floaters. A very large hemorrhage might block out all vision. See a short video on Viteous Hemorrhage.
It may take days, months or even years to resorb the blood, depending on the amount of blood present. If the eye does not clear the vitreous blood adequately within a reasonable time, vitrectomy surgery may be recommended. See a short video on Vitrectomy Surgery for Vitrous Hemorrhage.
Vitreous hemorrhage alone does not cause permanent vision loss. When the blood clears, visual acuity may return to its former level unless the macula is damaged.
Traction retinal detachment: When PDR is present, scar tissue associated with neovascularization can shrink, wrinkling and pulling the retina from its normal position. Macular wrinkling can cause visual distortion. More severe vision loss can occur if the macula or large areas of the retina are detached.
Neovascular glaucoma: Occasionally, extensive retinal vessel closure will cause new, abnormal blood vessels to grow on the iris (colored part of the eye) and block the normal flow of fluid out of the eye. Pressure in the eye builds up, resulting in neovascular glaucoma, a severe eye disease that causes damage to the optic nerve.
How is diabetic retinopathy diagnosed?
A medical eye examination is the only way to find changes inside your eye. An ophthalmologist (Eye M.D) can often diagnose and treat serious retinopathy before you are aware of any vision problems. The ophthalmologist dilates your pupil and looks inside of the eye with an ophthalmoscope.
If your ophthalmologist finds diabetic retinopathy, he or she may order color photographs of the retina or specialized retinal imaging called Optical Coherence Tomography (OCT) or a special test called fluorescein angiography to find out if you need treatment. In this later test, a dye is injected in your arm and photos of your eye are taken to detect where fluid is leaking.
Vision loss is largely preventable
If you have diabetes, it is important to know that today, with improved methods of diagnosis and treatment, only a small percentage of people who develop retinopathy have serious vision problems. Early detection of diabetic retinopathy is the best protection against loss of vision.
You can significantly lower your risk of vision loss by maintaining strict control of your blood sugar, knowing your A1C, and visiting your ophthalmologist regularly.
When to schedule an examination
People with diabetes should schedule examinations at least once a year. More frequent medical eye examinations may be necessary after the diagnosis of diabetic retinopathy.
Pregnant women with diabetes should schedule an appointment in the first trimester because retinopathy can progress quickly during pregnancy.
If you need to be examined for glasses, it is important that your blood sugar be in constant control for several days when you see your ophthalmologist. Glasses that work well when the blood sugar is out of control will not work well when sugar is stable.
Rapid changes in blood sugar can cause fluctuating vision in both eyes even if retinopathy is not present.
You should have your eyes checked promptly if you have visual changes that:
- Affect only one eye
- Last more than a few days
- Are not associated with a change in blood sugar
When you are first diagnosed with diabetes, you should have your eyes checked:
- Within five years of the diagnosis if you are 30 years old or younger;
- Within a few months of the diagnosis if you are older than 30 years.
Eye Works
Nonproliferative Diabetic Retinopathy
Cystoid Macular Edema
Macular Edema Injection and Laser
Proliferative Diabetic Retinopathy (PDR)
Macular Edema
Vitreous Hemorrhage
Vitrectomy for Vitreous Hemorrhage
Retinal Angiography
- Anatomy of the Eye
- Botox
- Cataracts
- Diabetes and the Eye
- Diabetic Retinopathy – What is it and how is it detected?
- Treatment for Diabetic Retinopathy
- Non-Proliferative Diabetic Retinopathy (NPDR) – Video
- Proliferative Diabetic Retinopathy (PDR) – Video
- Cystoid Macular Edema
- Vitreous Hemorrhage – Bleeding from diabetes (Video)
- Vitrectomy Surgery for Vitreous Hemorrhage (Video)
- Macular Edema
- Laser Procedures for Macular Edema (Video)
- Laser for Proliferative Diabetic Retinopathy – PDR (Video)
- How the Eye Sees (Video)
- Dilating Eye Drops
- Dry Eyes and Tearing
- Eye Lid Problems
- A Word About Eyelid Problems
- Bells Palsy
- Blepharitis
- Blepharoptosis – Droopy Eyelids (Video)
- Dermatochalasis – excessive upper eyelid skin (Video)
- Ectropion – Sagging Lower Eyelids (Video)
- Entropion – Inward Turning Eyelids (Video)
- How to Apply Warm Compresses
- Ocular Rosacea
- Removing Eyelid Lesions
- Styes and Chalazion
- Twitches or Spasms
- Floaters and Flashes
- Glaucoma
- Selective Laser Trabeculoplasty (SLT) for Glaucoma
- Glaucoma: What is it and how is it detected?
- Optical Coherence Tomography OCT – Retina & Optic Nerve Scan
- Treatment for Glaucoma
- Retinal Nerve Fibers and Glaucoma (Video)
- Open Angle Glaucoma (Video)
- Closed Angle Glaucoma (Video)
- Visual Field Test for Glaucoma
- Glaucoma and Blind Spots (Video)
- Treatment for Glaucoma with Laser Iridotomy (Video)
- Laser Treatment for Glaucoma with ALT and SLT (Video)
- Surgical Treatment for Glaucoma with Trabeculectomy (Video)
- Surgical Treatment of Glaucoma with Seton (Video)
- Keeping Eyes Healthy
- Laser Vision Correction
- Latisse for Eyelashes
- Macular Degeneration
- Macular Degeneration – What is it and how is it detected?
- Treatment for Macular Degeneration
- Dry Macular Degeneration (Video)
- Wet Macular Degeneration (Video)
- Treatment of Macular Degeneration with Supplements
- Treatment of Wet Macular Degeneration with Anti-VEGF Injections
- Amsler Grid – A home test for Macular Degeneration (Video)
- Living with Vision Loss
- How the Eye Works – The Macula (Video)
- Other Eye Conditions
- Central Serous Retinopathy
- Lattice Degeneration of the Retina
- A Word About Other Eye Conditions
- Amblyopia
- Carotid Artery Disease and the Eye
- Fuch’s Corneal Dystrophy
- Herpes Simplex and the Eye
- Herpes Zoster (Shingles) and the Eye
- Ischemic Optic Neuropathy
- Keratoconus
- Macular Hole
- Macular Pucker
- Microvascular Cranial Nerve Palsy
- Migraine and the Eye
- Optic Neuritis
- Pseudotumor Cerebri
- Retinal Vein Occlusion
- Retinitis Pigmentosa
- Retinopathy of Prematurity
- Strabismus
- Thyroid Disorders and the Eye
- Uveitis
- Vitreomacular Adhesions / Vitreomacular Traction Syndrome
- Red Eye
- Refractive Errors
- Retinal Tears and Detachments
Disclaimer
This Patient Education Center is provided for informational and educational purposes only. It is NOT intended to provide, nor should you use it for, instruction on medical diagnosis or treatment, and it does not provide medical advice. The information contained in the Patient Education Center is compiled from a variety of sources. It does NOT cover all medical problems, eye diseases, eye conditions, ailments or treatments.
You should NOT rely on this information to determine a diagnosis or course of treatment. The information should NOT be used in place of an individual consultation, examination, visit or call with your physician or other qualified health care provider. You should never disregard the advice of your physician or other qualified health care provider because of any information you read on this site or any web sites you visit as a result of this site.
Promptly consult your physician or other qualified health provider if you have any health care questions or concerns and before you begin or alter any treatment plan. No doctor-patient relationship is established by your use of this site.