Macular Hole
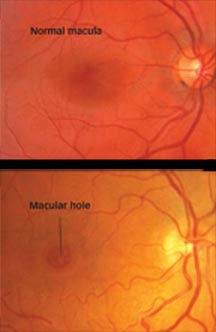
In the lower picture, note the round area of retinal tissue, missing in the center of the macula.
The macula is the central area of one of the most important parts of your eye; the retina.
The retina is a thin layer of light-sensitive tissue that lines the back of the eye. Light rays are focused onto the retina, where they are transmitted to the brain and interpreted as the images you see. The macula is the portion of the retina responsible for clear, detailed vision.
How does a macular hole form?
Your eye is filled with a gel-like substance called vitreous, which lies in front of the macula. As you age, the vitreous gel shrinks and pulls away from the macula, usually with no negative effect on your sight. In some cases, however, the vitreous gel sticks to the macula and is unable to pull away. As a result, the macular tissue stretches. After several weeks or months the macula tears, forming a hole. Less common causes of macular holes include injury and long-term swelling of the macula.
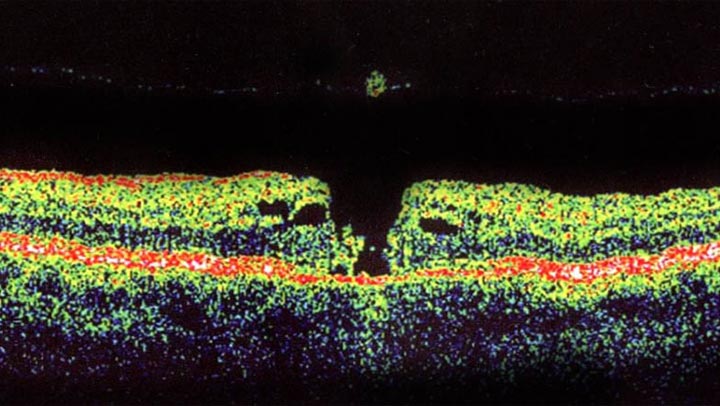
Cross-sectional image of macular hole. Note the missing piece of macula floating in the vitreous.
What are the symptoms of a macular hole?
In the early stages of hole formation, your central vision becomes blurred and distorted. If the hole progresses, a blind spot develops in your central vision and impairs the ability to see at both distant and close range.
It is important to note that if the macula is damaged, you will not lose your vision entirely. You will still have peripheral, or side, vision.
What tests will be performed?
Your ophthalmologist (Eye M.D.) will diagnose a macular hole by looking inside your eye with special instruments. Your ophthalmologist may use a test called optical coherence tomography, or OCT, to scan and examine your retina. OCT uses light waves to reveal specific layers of the retina.
How is a macular hole treated?
Vitrectomy surgery is the most effective treatment to repair a macular hole and possibly improve vision. The surgery involves using tiny instruments to remove the vitreous gel that is pulling on the macula. The eye is then filled with a special gas bubble to help flatten the macular hole and hold it in place while it heals.
You must maintain a constant face-down position after surgery to keep the gas bubble in contact with the macula. This can range from a few days to a few weeks, depending on your surgeon’s recommendation. A successful result often depends on how well this position is maintained. The bubble will then slowly dissolve on its own.
Do not fly in an airplane or travel at high altitudes until the gas bubble has dissolved. A rapid increase in altitude can cause a dangerous rise in eye pressure.
You can expect some discomfort after surgery. You will need to wear an eye patch for a short time. Your ophthalmologist will prescribe eyedrops for you and advise you when to resume normal activity.
As the macular hole closes, the eye slowly regains part of the lost sight. The outcome for vision may depend on the size of the hole and how long it was present before surgery. The amount of visual recovery can vary.
What are the risks of macular hole surgery?
Some of the risks of vitrectomy include:
- Infection of the eye
- Bleeding of the eye
- Retinal detachment
- High pressure in the eye
- Poor vision
- Accelerated cataract formation
It is important that you discuss the potential risks and benefits of this procedure with your ophthalmologist before making a decision regarding treatment.
Macular Hole
Macular Hole Surgery
Article Videos
- Anatomy of the Eye
- Botox
- Cataracts
- Diabetes and the Eye
- Diabetic Retinopathy – What is it and how is it detected?
- Treatment for Diabetic Retinopathy
- Non-Proliferative Diabetic Retinopathy (NPDR) – Video
- Proliferative Diabetic Retinopathy (PDR) – Video
- Cystoid Macular Edema
- Vitreous Hemorrhage – Bleeding from diabetes (Video)
- Vitrectomy Surgery for Vitreous Hemorrhage (Video)
- Macular Edema
- Laser Procedures for Macular Edema (Video)
- Laser for Proliferative Diabetic Retinopathy – PDR (Video)
- How the Eye Sees (Video)
- Dilating Eye Drops
- Dry Eyes and Tearing
- Eye Lid Problems
- A Word About Eyelid Problems
- Bells Palsy
- Blepharitis
- Blepharoptosis – Droopy Eyelids (Video)
- Dermatochalasis – excessive upper eyelid skin (Video)
- Ectropion – Sagging Lower Eyelids (Video)
- Entropion – Inward Turning Eyelids (Video)
- How to Apply Warm Compresses
- Ocular Rosacea
- Removing Eyelid Lesions
- Styes and Chalazion
- Twitches or Spasms
- Floaters and Flashes
- Glaucoma
- Selective Laser Trabeculoplasty (SLT) for Glaucoma
- Glaucoma: What is it and how is it detected?
- Optical Coherence Tomography OCT – Retina & Optic Nerve Scan
- Treatment for Glaucoma
- Retinal Nerve Fibers and Glaucoma (Video)
- Open Angle Glaucoma (Video)
- Closed Angle Glaucoma (Video)
- Visual Field Test for Glaucoma
- Glaucoma and Blind Spots (Video)
- Treatment for Glaucoma with Laser Iridotomy (Video)
- Laser Treatment for Glaucoma with ALT and SLT (Video)
- Surgical Treatment for Glaucoma with Trabeculectomy (Video)
- Surgical Treatment of Glaucoma with Seton (Video)
- Keeping Eyes Healthy
- Laser Vision Correction
- Latisse for Eyelashes
- Macular Degeneration
- Macular Degeneration – What is it and how is it detected?
- Treatment for Macular Degeneration
- Dry Macular Degeneration (Video)
- Wet Macular Degeneration (Video)
- Treatment of Macular Degeneration with Supplements
- Treatment of Wet Macular Degeneration with Anti-VEGF Injections
- Amsler Grid – A home test for Macular Degeneration (Video)
- Living with Vision Loss
- How the Eye Works – The Macula (Video)
- Other Eye Conditions
- Central Serous Retinopathy
- Lattice Degeneration of the Retina
- A Word About Other Eye Conditions
- Amblyopia
- Carotid Artery Disease and the Eye
- Fuch’s Corneal Dystrophy
- Herpes Simplex and the Eye
- Herpes Zoster (Shingles) and the Eye
- Ischemic Optic Neuropathy
- Keratoconus
- Macular Hole
- Macular Pucker
- Microvascular Cranial Nerve Palsy
- Migraine and the Eye
- Optic Neuritis
- Pseudotumor Cerebri
- Retinal Vein Occlusion
- Retinitis Pigmentosa
- Retinopathy of Prematurity
- Strabismus
- Thyroid Disorders and the Eye
- Uveitis
- Vitreomacular Adhesions / Vitreomacular Traction Syndrome
- Red Eye
- Refractive Errors
- Retinal Tears and Detachments
Disclaimer
This Patient Education Center is provided for informational and educational purposes only. It is NOT intended to provide, nor should you use it for, instruction on medical diagnosis or treatment, and it does not provide medical advice. The information contained in the Patient Education Center is compiled from a variety of sources. It does NOT cover all medical problems, eye diseases, eye conditions, ailments or treatments.
You should NOT rely on this information to determine a diagnosis or course of treatment. The information should NOT be used in place of an individual consultation, examination, visit or call with your physician or other qualified health care provider. You should never disregard the advice of your physician or other qualified health care provider because of any information you read on this site or any web sites you visit as a result of this site.
Promptly consult your physician or other qualified health provider if you have any health care questions or concerns and before you begin or alter any treatment plan. No doctor-patient relationship is established by your use of this site.